In Malaysia, road traffic accident is the main cause of maxillofacial trauma followed by falls, occupational injuries, inter-personal violence and sports injuries.
Injuries resulting from maxillofacial trauma ranges from simple bruises to extensive facial bone fractures which are often associated with injury to the brain.
The unique aspect of maxillofacial fractures is their impact on the dentition either directly or indirectly. Hence, maxillofacial trauma is one of the core procedures of the dentally qualified oral and maxillofacial surgeons.
Unlike the long bone, fractures of the face and jaw bones (maxillofacial bones) are more resistant to infection given its rich blood supply. On the other hand, maxillofacial fractures may cause profuse bleeding and obstruct air passages (airway)
One of the key factors in the treatment of maxillofacial fractures is restoration of facial dimensions, which is dependent on jaw relationship, that is in turn, guided by teeth relationship. Therefore restoring pre-trauma teeth relationship is pivotal in correcting jaw position and may also be used to prevent movement of the fractured jaw bones.
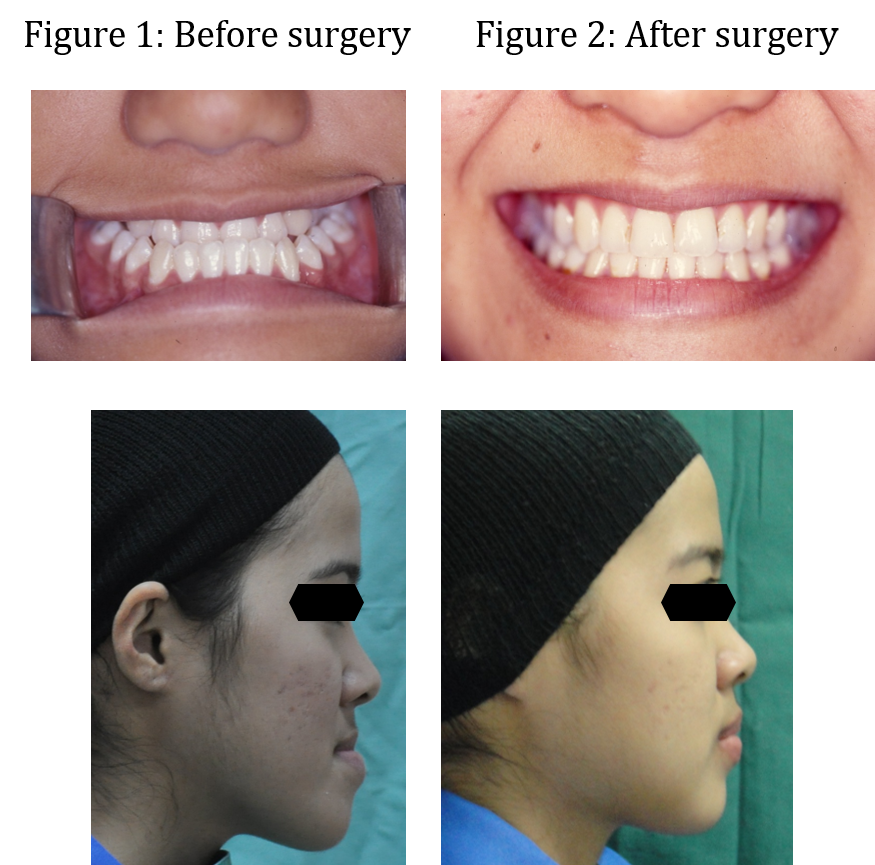
Maxillofacial fractures may be treated surgically with fixation of plates and screws (Figure 1) or non-surgically with fixation of wires around teeth and between upper and lower teeth (Figure 2). One of the advantages of surgical intervention is fast restoration of chewing function. Surgery is often inevitable for complicated fractures that disturbs function and deforms the face.
Figure 1: Surgical treatment of fractures with plates and screws
Figure 2: Non-surgical treatment of fractures with wires and elastic bands

Patients with acute maxillofacial fractures that present to the Trauma Centre will be referred to the Oral and Maxillofacial unit. Patients may also come directly to the dental faculty as out patient.
We also offer management of post trauma deformity and oral rehabilitation.
.jpg)